Medical Coders Who Do Not Learn AI Will Be Replaced Faster Than They Expect
Why CAIMC Is No Longer Optional for Career Survival
Posted by Medesun Global | 2026
The medical coding industry is undergoing its most disruptive transformation in decades. Artificial Intelligence is no longer an experiment or a future concept. It is already embedded in EHR systems, payer edits, risk adjustment analytics, denial engines, and audit platforms.
The uncomfortable truth is this:
Medical coders who do not understand AI will be replaced very fast.
Not by AI alone — but by AI-enabled coders.
The Harsh Reality Facing Medical Coders
Healthcare organizations today demand:
-
Faster turnaround times
-
Near-zero error rates
-
Audit-ready documentation
-
Predictive risk identification
-
Compliance across CMS, Medicare Advantage, and commercial payers
Manual coding alone cannot meet these demands anymore.
Hospitals, RCM companies, and Medicare Advantage plans are rapidly adopting:
-
AI-assisted coding engines
-
Automated HCC detection tools
-
Real-time denial prevention systems
-
NLP-based documentation analysis
Coders who only know traditional rule-based coding are increasingly viewed as slow, expensive, and high-risk.
AI Will Not Replace Coders — Coders Without AI Will Be Replaced
This distinction is critical.
AI systems still require:
-
Clinical judgment
-
Guideline interpretation
-
Compliance validation
-
CDI clarification
-
Audit defense
But they also require humans who understand how AI works.
The new demand is for AI-literate medical coders who can:
-
Validate AI-generated codes
-
Identify AI errors and hallucinations
-
Supervise automated workflows
-
Translate AI output into compliant claims
This is where the career divide begins.
What Happens to Coders Who Ignore AI?
Medical coders who resist AI face:
-
Shrinking job opportunities
-
Lower salary growth
-
Replacement by hybrid roles
-
Increased audit exposure
-
Reduced relevance in Medicare Advantage and inpatient coding
Employers are already preferring coders who can:
-
Work alongside AI
-
Audit AI-generated coding
-
Use AI for productivity and compliance
Ignoring AI today is equivalent to ignoring ICD-10 in 2015.
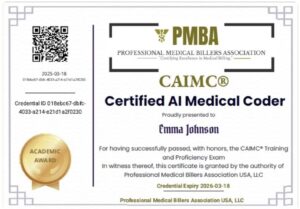
Why CAIMC Exists: Certified AI Medical Coder
CAIMC — Certified AI Medical Coder — was created to address this exact crisis.
CAIMC is not about replacing coding fundamentals.
It is about upgrading coders to survive and lead in the AI era.
CAIMC Trains Coders To:
-
Understand Agentic AI in medical coding
-
Perform AI-assisted ICD-10-CM, CPT, ICD-10-PCS coding
-
Validate auto-coded claims
-
Detect AI-driven coding risks
-
Support HCC and Medicare Advantage workflows
-
Generate compliant CDI queries using AI
-
Prepare for AI-based audits and OIG scrutiny
CAIMC turns coders into AI supervisors, not AI victims.
Salary and Job Security Are Already Shifting
Industry trends clearly show:
-
AI-enabled coders earn significantly more than manual coders
-
Hybrid coding roles are growing faster than traditional roles
-
Medicare Advantage and inpatient employers now expect AI familiarity
The future belongs to coders who can:
-
Code accurately
-
Audit confidently
-
Validate AI output
-
Protect organizations from compliance risk
CAIMC prepares coders for exactly this future.
The Timeline Is Shorter Than You Think
AI adoption in medical coding is accelerating faster than ICD-10 ever did.
Within the next few years:
-
Most routine coding will be AI-assisted
-
Manual abstraction roles will decline
-
Audit and validation roles will dominate
The question is not if AI will change your job.
The question is whether you will control AI or be replaced by someone who does.
Final Message to Medical Coders
Medical coding is not dying.
Outdated coding skills are.
The safest career path today is:
-
Learn AI
-
Work with AI
-
Supervise AI
-
Audit AI
CAIMC is not just a certification.
It is a career survival strategy.
Don’t Compete With AI. Learn to Control It.
Enroll in CAIMC – Certified AI Medical Coder
Only at Medesun Medical Coding Academy
🔗 Visit: medesunglobal.com